Covering more territory to fight resistance: considering nurses’ role in antimicrobial stewardship
Covering more territory to fight resistance: considering nurses’ role in antimicrobial stewardship
R Edwards1,* , LN Drumright 1 , M Kiernan 2,3 , A Holmes1,4
1. The National Centre for Infection Prevention and Management, Division of Infectious Diseases, Imperial College London, London, W12 OHS, UK. Email: [email protected]
2. Infection Prevention Society, UK
3. Southport and Ormskirk Hospital NHS Trust, UK
4. Imperial College Healthcare NHS Trust, London, UK
* Corresponding author
Accepted for publication: 6 October 2010
Key words: Antimicrobial resistance, nurse, healthcare associated infection, Clostridium difficile
Abstract
The potential contribution nurses can make to the management of antimicrobials within an in-patient setting could impact on the development of antimicrobial resistance (AMR) and healthcare associated infections (HCAIs). Current initiatives promoting prudent antimicrobial prescribing and management have generally failed to include nurses, which subsequently limits the extent to which these strategies can improve patient outcomes. For antimicrobial stewardship (AS) programmes to be successful, a sustained and seamless level of monitoring and decision making in relation to antimicrobial therapy is needed. As nurses have the most consistent presence as patient carers, they are in the ideal position to provide this level of service. However, for nurses to truly impact on AMR and HCAIs through increasing their profi le in AS, barriers and facilitators to adopting this enhanced role must be contextualised in the implementation of any initiative.
Over the past decade, there has been an increase in the prevalence of micro-organisms that are resistant to antimicrobial treatment. Antimicrobial resistance (AMR) is an increasing problem that limits and complicates treatment of infections – particularly in hospitals ( MacDougall and Polk, 2005 ). Initiatives have been implemented within acute care settings to promote prudent antibiotic prescribing that have primarily targeted the practices of pharmacists and doctors within this context.
Very little consideration has been afforded to the contribution nurses can make to the management of antimicrobials and how this may impact the development of AMR and healthcare associated infections (HCAIs). Herein we further discuss the problem and explore the extent to which nurses could contribute to the management of antimicrobials within an in-patient setting, while considering the difficulties inherent in introducing a new realm of responsibility to a workforce already challenged in time and resources.
The impact of antimicrobial therapy on acute healthcare
Excessive and indiscriminate use of antimicrobials in acute care settings contributes to the emergence and dissemination of antimicrobial resistant organisms, such as Meticillin-resistant Staphylococcus aureus (MRSA) and Vancomycin-resistant enterococci (VRE) ( Dancer, 2008 ; Taconelli et al, 2008 ). The spread of New Delhi metallo- β-lactamase (NDM) from the Asian subcontinent to Europe is just one recent reminder of the continuing evolution of AMR. This highlights potential for the spread of resistant organisms globally, promulgated by the connectivity of the world through air travel, and particularly through emerging trends in treatment options in the form of ‘medical tourism’ ( Kumarasamy et al, 2010 ). Thus the UK is not only vulnerable to AMR emerging as a result of local suboptimal practice, but also to the ramifications of poor antimicrobial management internationally.
Inappropriate antimicrobial use also results in an increased prevalence of HCAIs, such as Clostridium difficile infection (CDI) ( Barbut and Petit, 2001 ; Bartlet, 2008 ). More than 90% of CDI occurs following or during treatment with antibiotics, with CDI disproportionately affecting elderly patients ( Barbut and Petit, 2001 ; Weston, 2008 ). Signifi cant problems relating to antimicrobial therapy emerge in hospitals as many patients receive antimicrobials and are often highly susceptible to infections due to complex, severe illness and compromised immunity. When infections present in a single patient they can be transmitted to other patients and ultimately become endemic in hospital settings ( Weston, 2008 ). Furthermore, HCAIs caused by resistant organisms are associated with increased morbidity and mortality, and a longer hospital stay compared with infections caused by more sensitive organisms ( Cosgrove, 2006 ; Owens et al, 2008). The impact of HCAIs such as MRSA and CDI on patients’ experience of healthcare has been profound, with infection rates being one of the primary concerns of individuals being admitted to hospital ( Department of Health, 2004 ). Increased monitoring of antimicrobials combined with optimization of antibiotic prescribing and infection prevention and control strategies, have been shown to reduce HCAIs ( Dubberke et al, 2008 ). Further, judicious selection of antimicrobials and appropriate duration of therapy slows or prevents the emergence of resistant organisms ( Davey et al, 2005 ). Antimicrobial prescribing and management choices involve a multidimensional decision making process based on a fundamental understanding of the key principles of microbiology and the ramifi cations of inappropriate antibiotic use ( Charani et al, 2010). However it is estimated that between 25%–68% of antibiotic use in hospitals is inappropriate ( Dunagan et al, 1989 ; House of Lords, 1998 ; Behar et al, 2000 ; Willemsen et al, 2007 ), with many aspects of antimicrobial management having an impact on the emergence of AMR, HCAIs and patient outcomes. In addition to this, the highest incidence of medication errors occur during the administration of antibiotics (Lewis et al, 2009 ). Considering the link between the inappropriate use of antibiotics and the development of drug-resistant organisms and CDI, it is imperative that systems are implemented to optimise antimicrobial use in hospitals to decrease HCAIs and increase patient safety.
Nurses’ role in antimicrobial stewardship
Preventing further emergence of AMR depends on optimising use of antimicrobials through such activities as ensuring the agents used to treat infection are as specific as possible; courses of antibiotics being stopped at the earliest opportunity; oral rather than intravenous route of administration being used whenever appropriate; and some antibiotics being avoided in hospital settings ( Knox et al, 2002 ; MacDougall and Polk, 2005 ). Antimicrobial stewardship (AS) has been described as a multidisciplinary approach to minimising the development of AMR through selection of appropriate antimicrobials, optimising dose and duration, and minimising toxicity and side effects (Knox et al, 2002 ; MacDougall and Polk, 2005 ). Antimicrobial stewardship programmes (ASP) have been implemented throughout many UK hospitals, and although they are described as multidisciplinary in approach, nurse involvement in AS has been limited. AS teams have primarily included infectious disease physicians, clinical or infectious disease pharmacists, clinical microbiologists, and epidemiologists ( Lesprit and Brun-Buisson, 2008 ), and there is currently a lack of recognition of how nurses can contribute to the reduction of HCAIs and AMR through participation in ASP. It has been suggested that AS teams collaborate with infection control teams, including infection control nurses, however this is primarily for multidisciplinary data exchange (MacDougall and Polk, 2005 ), and the potential contribution nurses can make to the management of antimicrobials on the ward remains under-explored.
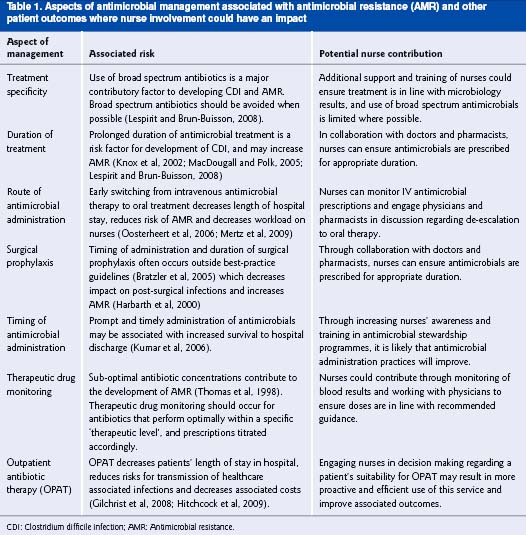
Currently, elements of AS such as monitoring duration and indication for antimicrobial treatment, instigating prompt de-escalation from intravenous to oral therapy, monitoring for drug allergies and side effects, monitoring therapeutic levels, ensuring timely administration of antimicrobials and following up on missed doses have primarily fallen into the work remit of physicians and pharmacists. However, owing to time constraints, workload and high staff rotation, it may be difficult for these activities to be performed consistently. Nurses work at multiple levels within the clinical setting, playing a key role in patient safety and have the most consistent presence as patient carers. With review of medication charts being part of routine professional practice and as the primary healthcare workers within the hospital setting to administer medications, nurses are in a key position to collaborate with AS teams and contribute to the multidisciplinary management of antimicrobials throughout acute care settings. Table 1 highlights some of the areas of antimicrobial management that nurses could impact upon, thus potentially making a valuable contribution to AS. Yet omission of nurses from decision making processes about antimicrobial therapy has limited the extent to which nurses may influence outcomes. In particular, antibiotic treatment decision making on general ward rounds, or on rounds targeted specifically at reviewing antimicrobial therapy are opportunities for nurses to make a contribution. Ward rounds can result in cooperative decision
making between nurses and other healthcare colleagues ( Beuscart-Zephir et al, 2005 ), and although generally not directly involved in prescribing, nurses can influence the decision making of medical and other prescribers through, for example, encouraging medication compliance, monitoring prescription decisions and reducing prescribing errors (Castledine, 2006 ; Jutel and Menkes, 2010 ). Nurse involvement in ward rounds could provide nurses, physicians and pharmacists with a venue for prompt dialogue to discuss antimicrobial treatment, indication, and duration, thus further enhancing the multidisciplinary management of AS to reinforce best practice. Ward nurses are also in a key position to facilitate patient referrals for outpatient antibiotic therapy in instances where patient admission to hospital is for extended antibiotic therapy only. This proactive approach to patient care could reduce patients’ length of stay, thus decreasing
their risk of HCAIs and associated costs, and enabling the patient to continue treatment in their own environment.
A collaborative approach to antimicrobial management
Nurses have already demonstrated that they can have a positive impact on patient outcomes in other specialty areas such as pain management, which in the past has been heavily based on medication use. Nurse introduction of non-pharmacological and patient education approaches to reduce pain has subsequently decreased patients’ reliance on medications ( Wells-Federman et al, 2002 ). It is possible that initiatives focused on increasing nurses’ participation in antimicrobial management activities can yield similar success. Although in the past there has been a focus on expanding the prescribing authority of nurses, which has become emblematic of professional autonomy, it may be more appropriate to look at the infl uence nurses may have in the management of drugs (Jutel and Menkes, 2010 ), and how this can be channelled to enhance AS.
Participation in the multidisciplinary management of antimicrobials would provide an avenue through which nurses could be more effective patient advocates. As specifi ed in the UK Code of Conduct for Nurses ( Nursing and Midwifery Council, 2007 ), nurses have an obligation to be patient advocates, ensuring that those in their care have access to relevant health care, information and support. As part of this function, the appropriate management and administration of antimicrobials is enshrined in nursing practice, and as such, nurses have a responsibility to ensure that antimicrobials are used appropriately, that administration of antimicrobials occurs in accordance with the treatment plan, and that any variations are acted on promptly to ensure optimal therapy. However, nurses’ exclusion from ASP has created an environment in which antimicrobial management is considered to be outside the remit of nursing responsibilities and expertise, which essentially has disempowered healthcare institutions from taking a true multidisciplinary approach to optimising antimicrobial use. Although the value in bringing together the expertise and experience of a variety of healthcare professionals may seem apparent, interprofessional collaboration is increasingly becoming a complex concept often marred by unclear working methods and a lack of understanding about how to translate knowledge into practice ( San Martin-Rodriguez, 2005 ). However, it is understood that a hospital’s success and patient outcomes are strongly dependent on how effectively the members work together as a team ( Rafferty et al, 2001 ; Leonard et al, 2004 ).
Therefore, it is likely that effective monitoring and direct communication between healthcare professionals, including nurses, regarding antimicrobial use would promote best practice, improve patient care and reduce nurses’ workload. Specifically, these activities are likely to contribute to reducing the risk of CDI and HCAIs associated with antimicrobial
use, thus decreasing patient morbidity and mortality, reducing length of stay and improving patient experience of health care. Although it is recognised that expertise is required to manage antimicrobial treatment, in reality the decision making process is often performed by junior doctors working outside their area of expertise with varying levels of senior support ( Charani et al, 2010 ).
The high rotation of junior doctors throughout wards means that a repository for local knowledge about the management of antimicrobials for specific patient groups is lost. Prescribing and management of antimicrobials occurs across all areas of healthcare and does not sit within a particular specialty, and as such the memory of the healthcare organisation suffers. Organisational memory refers to the retrievable information contained within an organisation in formats such as spreadsheets and guidelines as well as in the minds of the organization members ( Paoli and Prencipe, 2003 ). As one of the less transient professional populations within the hospital, nurses are in an ideal position to contribute to organisational memory regarding antimicrobial management.
In collaboration with physicians and pharmacists, nurses’ local knowledge could assist in informing decision choices in relation to antimicrobial therapy, and enhance the multidisciplinary approach to antimicrobial management. For ASP to continue to be successful, a sustained and seamless level of monitoring and decision making in relation to antimicrobial therapy is needed, and as the most consistent provider of care at the bedside, nurses are in the ideal position to provide this level of service.However, all nurses may not have the required training or profile among peers and other medical staff to actively contribute to antimicrobial management. Additionally, nursing shortages may impose time constraints that prohibit any additional duties into nurses’ work regimes. It is therefore important to fi rst assess the feasibility of increasing nurses’ participation in AS. It is necessary to identify what role nurses currently have in relation to the management of antimicrobials, and where this could be developed in the future.
Contextual challenges in the multidisciplinary management of antimicrobials
Assumptions that healthcare professionals have the time, resources, knowledge, motivation and skills to change clinical practice in line with evidence-based recommendations are counterproductive. Historically, interventions that focused on changing the behaviours of healthcare professionals have had limited success ( Cook et al, 2000 ; Pittet, 2004 ; Ferlie et al, 2005 ), especially if not implemented with an understanding of the cultural, contextual and environmental influences on professional practice. In order to more successfully engage healthcare workers in initiatives and produce more successful outcomes, the obstacles and facilitators to changing or adopting new practice must be considered in the development and implementation of any programme ( Hulscher et al, 2010 ). Therefore, for nurses to truly have an impact on AMR and HCAIs through increasing their profile in AS, barriers and facilitators to adopting this enhanced role must be contextualised. Furthermore, a clear understanding of nurses’ roles, and clarity among healthcare professionals of where responsibilities lie, will assist with cohesiveness among multidisciplinary teams. It would be remiss not to acknowledge the professional challenges that may be presented when attempting to enhance nurses’ role in antimicrobial management. Nurses’ ability to discuss or even challenge antimicrobial management choices is heavily connected to the construct of power and knowledge, particularly within the acute care context. Nurses may not feel they are in a position to participate in ASP due to lack of knowledge, closely linked to positions of power, particularly within healthcare environments ( Hindess, 1996 ). The challenges associated with influencing antimicrobial management decisions are further complicated through prescribing etiquette, which refers to prescribers’ reluctance to change colleagues’ decisions ( Lewis and Tully, 2009 ). Indeed, one could argue that moving away from the persistent use of the term ‘antimicrobial prescribing’ to antimicrobial management would facilitate a more inclusive approach. The term ‘prescribing’ relates to a specific area of expertise associated primarily with the practice of doctors and pharmacists, eliminating nursing from the decision making process. Acknowledging that it is the management of antimicrobials that leads to the emergence of AMR and HCAIs could facilitate a more holistic approach to ensuring antimicrobials are used appropriately and could facilitate nurses’ involvement in ASP.
Conclusion
Given the increasing social and economic burden of AMR and HCAIs, it is critical that healthcare professionals increase their efforts to work together across disciplines for the protection and safety of their patients. The implementation of ASP within the UK has been effective in promoting prudent antimicrobial prescribing, however the extent to which nurses can contribute to such initiatives is poorly understood. As the most consistent providers of care at the bedside, and because medication chart review is part of their routine professional practice, nurses are in an ideal position to enhance antimicrobial management through multidisciplinary collaboration. Increasing nurses’ awareness of antimicrobial use and the impact of antibiotic therapy on infection outcomes is likely to enhance the optimisation of antimicrobial treatment, monitoring and administration. Nurse involvement in AS could therefore be a time- and cost-efficient use of resources while improving patient safety and quality of care. As pharmacological options for the treatment of infection decrease, and development of new antimicrobials is slow, it is imperative that initiatives to reduce AMR are implemented. For these initiatives to positively and sustainably impact on outcomes, it is necessary to gain a contextual understanding of the barriers and facilitators to nurses contributing to AS, and how this aspect of the nursing role may be developed in the future.
Acknowledgements
The authors acknowledge the support from the National Institute for Health Research (NIHR) Biomedical Research Centre Funding Scheme at Imperial College and the support from the National Centre for Infection Prevention and Management (CIPM) funded by the UK Clinical Research Collaboration.
Confl ict of interests
None declared.
References
Barbut F , Petit JC . ( 2001 ) Epidemiology of Clostridium difficile –associated infections . Clinical Microbiology and Infection 61: 246 – 53 .
Bartlet JG . ( 2008 ) Historical perspectives on studies of Clostridium difficile and C. difficile infection. Clinical Infectious Diseases 46 ( Suppl1 ): S4 – S11 .
Behar P , Wagner MB , Freitas I , Auler A , Selistre L , Fossatti L , Asquidamini S . ( 2000 ) Assessing the antimicrobial prescription request process in a teaching hospital in Brazil: regulations and training . Brazilian Journal of Infectious Diseases 4(2): 76 – 85 .
Beuscart-Zephir , MC , Pelayo S , Anceaux F , Meaux JJ , Degroisse M , Degoulet P . ( 2005 ) Impact of CPOE on doctor-nurse cooperation for the medication ordering and administration process . International Journal of Medical Informatics 74(7): 629 – 41.
Bratzler DW , Houck PM , Richards C , Steel L , Dellinger P , Fry DE , Wright C , Ma A , Carr K , Red L . ( 2005 ) Use of antimicrobial prophylaxis for major surgery: baseline results from the national surgical infection prevention project . Archives of Surgery 140(2): 174 – 82 .
Castledine G . ( 2006 ) Prescribing is not the only issue for nurses and drugs , British Journal of Nursing 15 ( 15) : 836 – 7 .
Charani E , Cooke J , Holmes A . ( 2010 ) Antibiotic stewardship programmes – what’s missing? J ournal of Antimicrobial Chemotherapy 65 : 2275-7 .
Cook D , Ricard JD , Reeve B , Randall J , Wigg M , Brochard L , Dreyfuss D . ( 2000 ) Ventilator circuit and secretion management strategies: a Franco-Canadian survey . Critical Care Medicine 28(10 ): 3547 – 54 . Cosgrove S . ( 2006 ) The relationship between antimicrobial resistance and patient outcomes , Clinical Infectious Diseases 42 ( Suppl 2) : S82 – S89 .
Dancer SJ . ( 2008 ) The effect of antibiotics on methicillin-resistant Staphylococcus aureus. Journal of Antimicrobial Chemotherapy 61(2): 246 – 53 .
Davey P , Brown E , Fenelon L , Finch R , Gould I , Hartman G , Holmes A , Ramsay C , Taylor E , Wilcox M , Wiffen PJ . ( 2005) Interventions to improve antibiotic prescribing practices for hospital inpatients . Cochrane Database of Systematic Reviews 2005, Issue 4 . John Wiley & Sons, Ltd . Department of Health ( 2004 ) Towards cleaner hospitals and lower rates of infections: a summary of action. Department of Health : London .
Dubberke E , Gerdin D , Classen D , Arias K , Podgorny K , Anderson D , Burstin H , Calfee DP , Coffi n SE , Fraser V , Griffin FA , Gross P , Kaye K , Klompas M , Lo E , Marschall J , Mermel LA , Nicolle L , Pegues DA , Perl TM , Saint S , Salgado CD , Weinstein , RA , Wise R , Yokoe D . ( 2008 )
Strategies to prevent Clostridium difficile infections in acute care hospitals, Infection Control and Hospital Epidemiology 29: S81 – S92 .
Dunagan EC , Woodward RS , Medoff G , Gray JL , Casabar E , Smith MD , Lawrenz CA , Spitznagel E . ( 1989 ) Antimicrobial misuse in patients with positive blood cultures . A merican Journal of Medicine 87( 3 ):253 – 9 .
Ferlie E , Fitzgerald L , Wood M , Hawkins C . ( 2005 ) The nonspread of innovations: the mediating role of professionals. A cademy of Management Journal 48 ( 1 ): 117 – 34 .
Gilchrist M , Dean B , Patel J . ( 2008 ) An outpatient parenteral antibiotic therapy (OPAT) map to identify risks associated with an OPAT service. Journal of Antimicrobial Chemotherapy 62: 177 – 83 .
Harbarth S , Samore MH , Lichtenberg D , Carmeli Y . ( 2000 ) Prolonged antibiotic prophylaxis after cardiovascular surgery and its effect on surgical site infections and antimicrobial resistance . Circulation 101:2916 – 21 .
Hindess B . ( 1996 ) Discourses of power: from Hobbes to Foucault. Blackwell Publishers : Oxford .
Hitchcock J , Jepson AP , Main J , Wickens HJ . ( 2009 ) Establishment of an outpatient and home parenteral antimicrobial therapy service at a London teaching hospital: a case series. Journal of Antimicrobial Chemotherapy 64 (3 ): 630 – 4 .
House of Lords Select Committee on Science and Technology. (1998) Resistance to antibiotics and other antimicrobial agents. Session 1997-98. 7th Report. London: The Stationery Office.
Hulscher M , Grol R , Meer J . ( 2010 ) Antibiotic prescribing in hospitals: a social and behavioural scientifi c approach . Lancet Infectious Diseases 10: 167 – 75 .
Jutel A , Menkes DB . ( 2010 ) Nurses’ reported infl uence on the prescription and use of medication . International Nursing Review 57( 1 ):
92 – 7 . Knox K , Lawson W , Dean Franklin B , Holmes A . ( 2002 ) Multidisciplinary antimicrobial management and the role of the infectious diseases pharmacist – a UK perspective . Journal of Hospital Infection 53( 2 ): 85 – 90 .
Kumar A , Roberts D , Wood K , Light B , Parrillo JE , Sharma S , Suppes R , Feinstein D , Zanotti S , Taiberg L , Gurka D , Kumar A , Cheang M . ( 2006 ) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock . Critical Care Medicine 34(6): 1589 – 96 .
Kumarasamy KK , Toleman MA , Walsh TR , Bagaria J , Butt F , Baladrishnan R , Chaudhary U , Doumith M , Giske CG , Irfan S, Krishnan P , Kumar AV , Maharjan S , Mushtaq S , Noorie T , Paterson DL , Pearson A , Perry C , Pike R , Rao B , Ray U , Sarma JB , Sharma M, Sheridan E , Thirunarayan MA , Turton J , Upadhyay S , Warner M , Welfare W , Livermore D , Woodford N . ( 2010 ) Emergence of a new antibiotic resistance mechanism in India, Pakistan, and the UK: a molecular, biological, and epidemiological study . Lancet Infectious Diseases 10(9): 597 – 602 .
Leonard M , Graham S , Bonacum D . ( 2004 ) The human factor: the critical importance of effective teamwork and communication in providing safe care . Quality and Safety in Health Care 13(Suppl 1 ): i85 – i90 .
Lesprit P , Brun-Buisson C . ( 2008 ) Hospital antibiotic stewardship . Current Opinion in Infectious Diseases 21: 344 – 9 . Lewis PJ , Tully MP . ( 2009 ) Uncomfortable prescribing decisions in hospitals: the impact of teamwork . Journal of the Royal Society of Medicine 102(11 ): 481 – 8 .
Lewis PJ , Dornan T , Taylor D , Tully M , Wass V , Ashcroft D . ( 2009 ) Prevalence, incidence and nature of prescribing errors in hospital inpatients: a systematic review . Drug Safety 32 : 379 – 89 . MacDougall C , Polk R . ( 2005 ) Antimicrobial stewardship programs in health care systems . Clinical Microbiology Reviews 18 (4): 638 – 56 . Mertz D , Koller M , Haller P, Lampert M , Plagge H , Hug B , Hug B , Koch G , Battegay M , Fluckiger U , Bassetti S . ( 2009 ) Outcomes of early switching from intravenous to oral antibiotics on medical wards . Journal of Antimicrobial Chemotherapy 64 ( 1 ): 188 – 99 . Nursing and Midwifery Council ( 2007 ) The Code: standards of performance, conduct and ethics for nurses and midwifes . Nursing and Midwifery Council : London .
Oosterheert J , Bonten M , Schneider M , Buskens E , Lammers J , Hustinx W , Kramer M , Prins JM , Slee P , Kaasjager K , Hoepelman A . ( 2006 )
Effectiveness of early switch from intravenous to oral antibiotics in severe community acquitted pneumonia: multicentre randomized trial . British Medical Journal 333: 1 – 5 .
Owens JC , Donskey CJ , Gaynes RP , Loo VG , Muto CA . ( 2008 ) Antimicrobial-associated risk factors for Clostridium difficile infection. Clinical Infectious Diseases 46(S1 ): S19 – S31 .
Paoli M , Prencipe A . ( 2003 ) Memory of the organisation and memories within the organisation . Journal of Management and Governance 7 ( 2 ): 145 – 62 .
Pittet D . ( 2004 ) The Lowbury Lecture: behaviour in infection control . Journal of Hospital Infection 58: 1 – 13 .
Rafferty AM , Ball J , Aiken LH . ( 2001 ) Are teamwork and professional autonomy compatible, and do they result in improved hospital care? Quality in Health Care 10 (Suppl II): ii32 – ii37 .
San Martin-Rodriguez LS , Beaulieu M , D’Amour D , Ferrada-Videla M . ( 2005 ) The determinants of successful collaboration: a review of theoretical and empirical studies . Journal of Interprofessional Care 19(s1 ): 132 – 47 .
Tacconelli E , De Angelis G , Cataldo MA , Pozzi E , Cauda R . ( 2008 ) Does antibiotic exposure increase the risk of methicillin-resistant Staphylococcus aureus (MRSA) isolation? A systematic review and meta-analysis . Journal of Antimicrobial Chemotherapy 61(1): 26 – 38 .
Thomas JK , Forrest A , Bhavnani SM , Hyatt JM , Cheng A , Ballow CH , Schentag JJ . ( 1998 ) Pharmacodynamic evaluation of factors associated with the development of bacterial resistance in acutely ill patients during therapy . A ntimicrobial Agents and Chemotherapy 42(3): 521 – 7 .
Wells-Federman C , Arnstein P , Caudill M . ( 2002 ) Nurse-led pain management program: effect of self-effi cacy, pain intensity, pain related disability, and depressive symptoms in chronic pain patients . Pain Management Nursing 3 ( 4 ): 131 – 40 .
Weston D . ( 2008 ) Infection prevention and control: theory and practice for healthcare professionals . John Wiley & Sons Ltd : Chichester . Willemsen I , Groenhuijzen A , Bogaers D , Stuurman A , Keulen P , Kluytmans J . ( 2007 ) Appropriateness of antimicrobial therapy measured by repeated prevalence surveys. A ntimicrobial Agents and Chemotherapy 51 ( 3 ): 864 – 7.



